Health & Wellbeing
Our experts show you simple and effective ways to stay healthy and active, so you can live your passions every day.

Vitamin D: are you taking the right kind?
We explain the difference between D2 and D3 and if a higher dose is always better.

The 7 signs you need a new pillow
Sleep experts say a worn out pillow could be sabotaging your sleep.

RSV vaccine: over 80s can finally get their free jab
At last – people over 80 are eligible for the RSV vaccine after a government change of heart.

How I helped rebuild my mum and dad
Rhoda and Michael Stephen were facing increasing ailments and a lack of mobility in their eighties. Until they took up weightlifting.
How our brains change at 66 and 83
We examine the science and how to best look after our brain as we get older.

I tried fermented food for a month and this is what happened
Is eating fermented good for you? Our writer gave it a go for four weeks, with some mixed results.

9 lifestyle changes that may cut your risk of Parkinson’s
Can you do anything to reduce your risk, or slow it down if you already have it?

Unlock better sleep: These seven changes transformed my nights

Breads ranked best to worst
We've ranked the main types of bread from best to worst - find out which is the healthiest and which to avoid.

5 easy ways to improve your sleep while you're awake
One of the UK's top sleep experts has simple changes to make to your waking hours which will transform your sleep.

I tried the new hearing glasses
We try out a pair of audio glasses to see whether they really do help your hearing.

Is skipping breakfast bad for your health?
We ask the experts to separate the fact from the fiction about the first meal of the day.
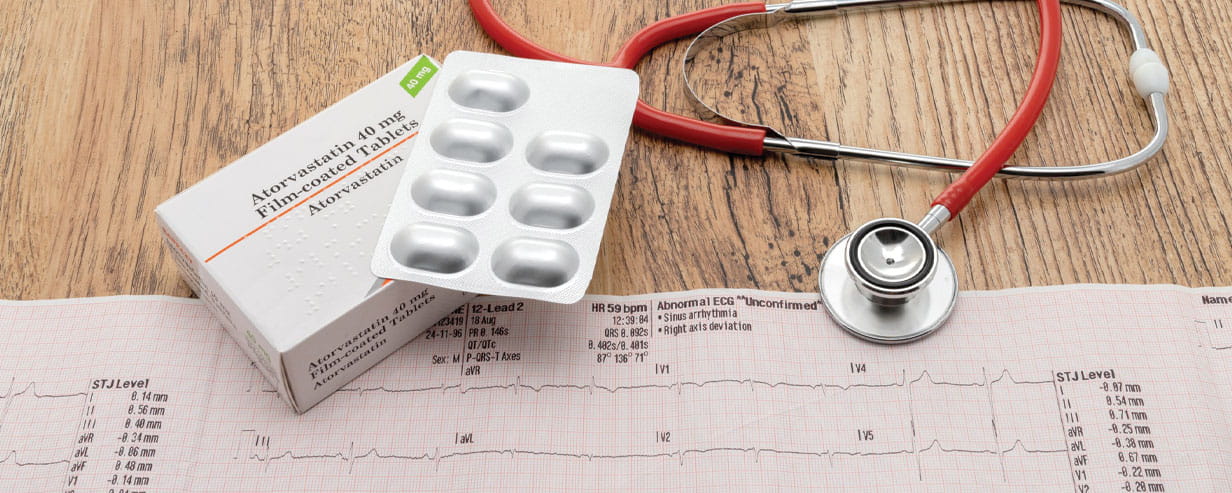
Everything you need to know about statins
Statins are safer than you think, and the benefits may grow as you age.

Do dogs make you healthier? A world-leading gut expert thinks so
Tim Spector explains how dogs support our gut health.

For a limited time, enjoy 3 issues of Saga Magazine for just £1. Receive the next 3 print editions delivered direct to your door, plus 3 months’ unlimited access to the Saga Magazine app—perfect for reading on the go.
Don’t miss your chance to experience award-winning content at an exceptional price.
Play our free daily puzzles
Beat the boredom and exercise your mind with our selection of free puzzles.